Diabetes isn’t just about sugar; it can quietly erode your chances of conceiving
Thu 30 Oct 2025, 01:27:24

In India, where the burden of diabetes is rising steadily, one less-talked-about complication is taking root: the impact of elevated blood sugar levels on fertility. Both men and women are seeing how diabetes and its underlying metabolic disturbances can quietly undermine their ability to conceive, often before they realise it.
The prevalence of diabetes in India has soared in recent decades. At the same time, fertility challenges are increasingly becoming part of the reproductive health conversation. What remains less recognised is how diabetes contributes directly to reproductive dysfunction.
What happens to women’s fertility when diabetes strikes
According to Dr Jasneet Kaur, Consultant and Clinical Director - Reproductive Medicine, Milann Fertility Hospital, Chandigarh, for women, diabetes—particularly type 2 diabetes (T2DM)—and insulin resistance can interfere with ovulation, hormone balance, and the quality of the eggs themselves.
These metabolic disturbances often overlap with polycystic ovary syndrome (PCOS), a common condition linked to both insulin resistance and subfertility. Women with PCOS are at a higher risk of developing prediabetes or diabetes later in life, and conversely, women with diabetes may show features of PCOS, creating a vicious cycle that worsens both reproductive and metabolic outcomes.
In both conditions, hyperinsulinaemia and chronic inflammation disrupt normal ovarian function. This can lead to irregular cycles, anovulation, and poor egg quality, making conception difficult. Insulin resistance, often a precursor or companion to diabetes, has been observed in nearly one-fifth of infertile women in some Indian studies; among those affected, pregnancy rates after ovulation induction are significantly lower.
The mechanisms are multifaceted: chronic hyperglycaemia triggers oxidative stress, glycation of proteins, inflammation, and hormonal imbalances. These in turn can lead to irregular menstruation, reduced uterine receptivity, and suboptimal embryo implantation. In short, for women, diabetes and insulin resistance can silently erode fertility long before obvious symptoms appear.
Moreover, insulin resistance, often a precursor or companion to diabetes, was found in 20.5 % of infertile women in one cohort; among those with insulin resistance, the pregnancy rate after ovulation induction was just 5.8 % compared to higher rates in women without it.
The mechanisms are multifaceted: chronic hyperglycaemia triggers oxidative stress, glycation of proteins, inflammation and hormonal disruptions. These in turn can lead to irregular menstruation, anovulation,
reduced egg quality and diminished uterine receptivity. In short, for women, diabetes can erode fertility long before obvious symptoms set in.
reduced egg quality and diminished uterine receptivity. In short, for women, diabetes can erode fertility long before obvious symptoms set in.
How diabetes impacts male fertility and sperm health
Men, too, are not spared. Diabetes impacts sperm quality, motility, and even increases DNA fragmentation in sperm cells. A study of semen parameters found that in diabetic men, semen volume (r = –0.28), sperm count (r = –0.22) and motility (r = –0.23) all showed weak but statistically significant negative correlations with blood sugar levels.
In addition, diabetic neuropathy can lead to retrograde ejaculation; vascular damage and oxidative stress may impair spermatogenesis; and erectile dysfunction (which is more common in men with diabetes) can also reduce chances of conception.
Why the link between diabetes and infertility remains unspoken
Part of the problem is awareness. Many couples undergoing fertility evaluation do not realise that an underlying metabolic condition like diabetes may be the root cause. The notion of ‘infertility’ often centres on structural or hormonal problems, while metabolic health gets overlooked.
What couples can do to protect their fertility
. Screen early: Both partners should have blood sugar/insulin-resistance screening when fertility issues arise.
. Importance of Glycaemic control: For women with T2DM, controlling glycemia may help to preserve ovarian function.
. Lifestyle changes: Diet, exercise, weight management and sleep quality can altogether improve insulin sensitivity and thus fertility outcomes.
. Fertility is not just a structural problem: When you find continuous failure in fertility even after treatments, check for metabolic factors like diabetes or insulin resistance for both men and women.
The Indian context: Fertility and the rising tide of diabetes
While the global data are mounting, Indian-specific studies are still limited. What is clear, however, is that the rising tide of metabolic disorders in urban India may be silently contributing to the growing burden of infertility. For instance, nearly one in five infertile women in a study exhibited insulin resistance.
Diabetes may often be thought of as a disease of the pancreas, heart, kidneys or eyes, but its reach extends quietly into the realm of fertility. Recognising it early, screening both partners, and addressing metabolic health proactively could make the difference between waiting and conceiving. For couples longing for a baby, this silent factor might just hold the key to unlocking success.
No Comments For This Post, Be first to write a Comment.
Most viewed from Health
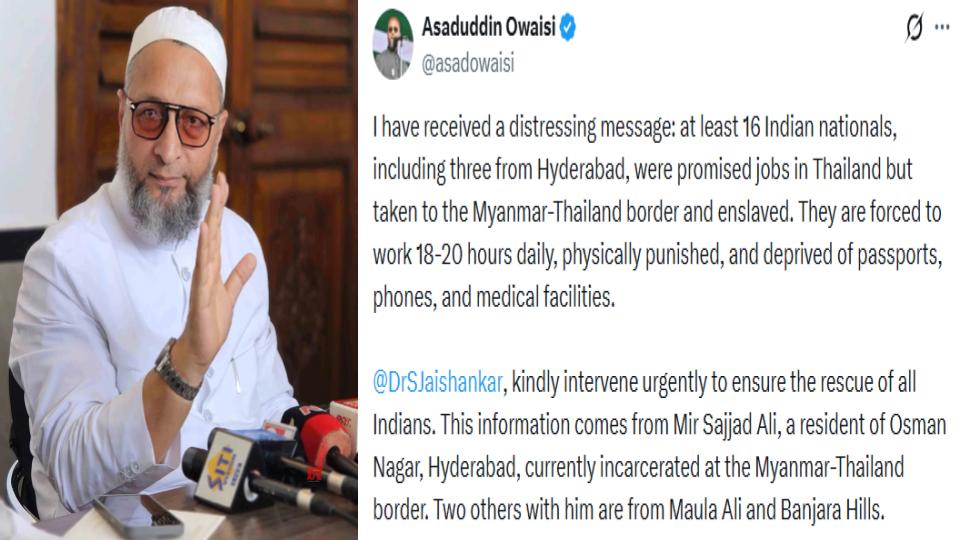
AIMIM News
Latest Urdu News
Most Viewed
May 26, 2020
Is it right to exclude Bangladesh from the T20 World Cup?
Latest Videos View All
Like Us
Home
About Us
Advertise With Us
All Polls
Epaper Archives
Privacy Policy
Contact Us
Download Etemaad App
© 2026 Etemaad Daily News, All Rights Reserved.




















.jpg)
.jpg)
.jpg)


